The Workforce and Cost Dilemma: How Healthcare Leaders Can Navigate Challenges Through Enterprise Transformation
In 2025, the healthcare industry stands at a pivotal moment. The twin pressures of workforce shortages and escalating costs threaten to destabilize its foundation. These challenges extend beyond operational hurdles to create risks for patient care quality and the sustainability of healthcare growth worldwide.
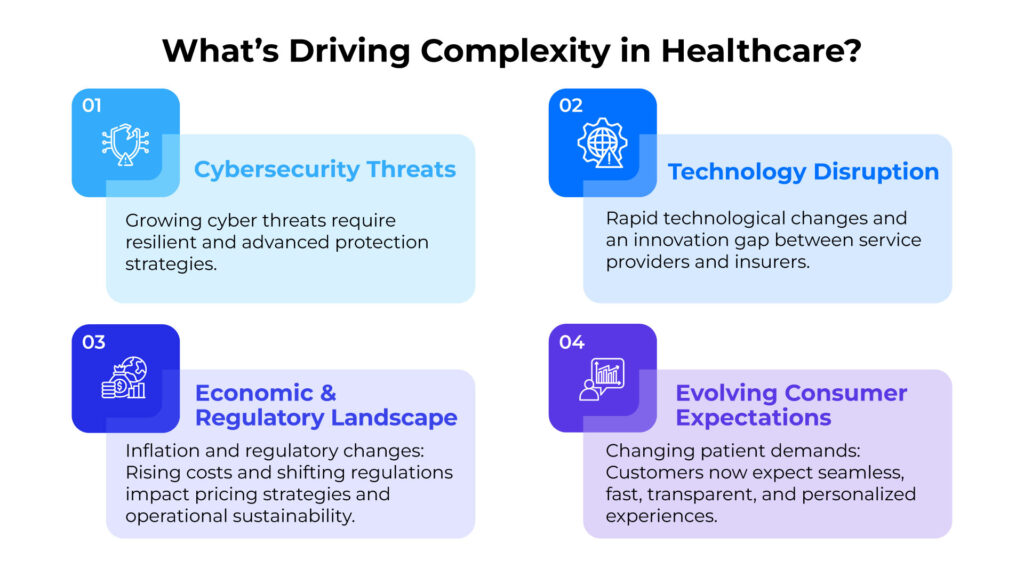
The healthcare landscape is growing increasingly complex. Persistent cybersecurity vulnerabilities, the rapid pace of technological change, gaps in innovation between insurers and providers, and intensifying pressures from inflation and regulatory shifts all contribute to this complexity. When combined with evolving patient expectations, healthcare leaders find themselves navigating unprecedented uncertainty and change.
Yet this period of disruption contains remarkable opportunities. Visionary organizations are turning to enterprise transformation as a solution. This approach represents a comprehensive reinvention of clinical practices, operational workflows, and technological ecosystems. By harnessing advanced innovations like generative AI, predictive analytics, robotic surgery, and blockchain technology, healthcare providers can redefine care delivery, strengthen system resilience, and create unprecedented value for patients and stakeholders.
This moment calls for courageous leadership and strategic vision. The healthcare industry isn’t merely approaching a crossroads—it stands on the threshold of a transformative evolution that will shape its trajectory for decades.
Breaking Point: The Dual Crisis of Workforce Shortages and Skyrocketing Costs
1. Workforce Shortages: An Urgent and Growing Problem
Healthcare faces a projected global deficit of 10 million workers by 2030, driven by burnout, an aging workforce, and rising care demands. The situation in the United States mirrors this global challenge:
- Nursing Shortages: By 2031, the U.S. will experience a deficit of 195,400 nurses, with rural communities bearing the heaviest impact.
- Physician Shortages: A potential gap of 124,000 physicians could emerge by 2033, particularly affecting primary care.
- Burnout: Nearly 3 in 10 healthcare workers are considering leaving the profession due to stress and unsustainable workloads.
- Consequences: Understaffed facilities compromise care quality, extend wait times, and drive operational costs higher.
2. Rising Costs: The Financial Strain
Centers for Medicare & Medicaid Services (CMS), Office of the Actuary, projected that overall U.S. healthcare spending will grow at an average annual rate of 5.4% from 2023 to 2032. By 2032, total healthcare spending is expected to reach $7.2 trillion, accounting for 19.7% of the national GDP.
- Inflationary Pressures: Rising prices of supplies, medications, and labor.
- Behavioral Health: Spending on mental health services has significantly increased since the pandemic.
- Temporary Staffing Solutions: Hospitals increasingly rely on expensive temporary workers to fill personnel gaps, further straining budgets.
- Consequences: These financial pressures force healthcare providers to make difficult choices between investing in quality care and maintaining financial viability.
Enterprise Transformation: A Strategic Lifeline for Healthcare’s Future

The challenges of workforce shortages and rising costs, while daunting, can be addressed through comprehensive enterprise transformation. This approach offers sustainable solutions that can reshape the healthcare landscape.
1. Leveraging Digital Technologies
Enterprise transformation provides scalable solutions to the pressing issues of workforce shortages and cost pressures:
- Telemedicine and Remote Monitoring: These technologies extend care access to underserved areas and reduce hospital readmissions by 25%. Providence Health, for example, expanded its telehealth services to reach 30% more rural patients while cutting readmission rates significantly.
- Artificial Intelligence (AI): AI streamlines administrative tasks and enhances diagnostic accuracy, detecting diseases like cancer with 95% accuracy. The Mayo Clinic’s implementation of AI in radiology has reduced diagnostic time by 30% while improving accuracy.
- Predictive Analytics: These tools optimize staffing levels and reduce readmission rates by 20%, eliminating unnecessary costs. UnitedHealth has successfully deployed predictive models that identify high-risk patients before complications arise.
- Blockchain and Cloud Computing: These technologies secure patient data and improve interoperability across systems. Estonia’s national healthcare system demonstrates the potential, creating a secure, unified health record accessible to authorized providers nationwide.
2. Building Resilient Workforces
To address burnout and retention challenges, forward-thinking organizations are implementing multifaceted strategies:
- Upskilling Staff: Training healthcare workers to effectively use AI and digital tools enhances efficiency and job satisfaction. Cleveland Clinic’s digital education program has improved retention rates by 15% while preparing staff for technology-enhanced care delivery.
- Flexible Work Models: Offering remote and hybrid roles improves work-life balance and expands the talent pool. Kaiser Permanente has reduced administrative burnout by 22% through flexible scheduling options.
Thailand’s Healthcare Revolution: A Model of Digital Innovation
Thailand offers a compelling case study in healthcare transformation, demonstrating how developing economies can leverage technology to overcome traditional barriers.
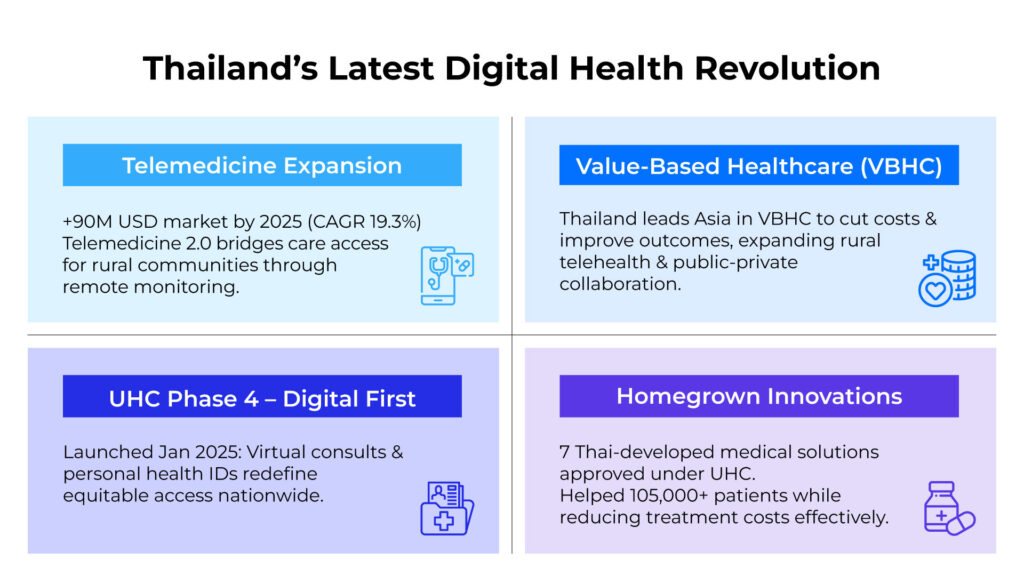
Telemedicine Expansion: Bridging the Urban-Rural Healthcare Divide
According to Frost & Sullivan (2024), Thailand’s telemedicine market is set to reach $90 million by 2025, growing at 19.3% annually—outpacing the Southeast Asian average of 14.6%.
The Telemedicine 2.0 initiative marks a paradigm shift from basic video consultations to an integrated patient data ecosystem. This platform leverages wearable devices, seamlessly connects with Electronic Medical Records (EMR), and employs advanced analytics for evidence-based remote treatment protocols.
This technology particularly benefits Thailand’s rural communities, where the physician-to-patient ratio is 1:5,000 compared to 1:800 in Bangkok, directly addressing a critical healthcare equity challenge.
Universal Health Coverage (UHC) Phase 4: A Digital-First Approach
In January 2025, Thailand launched UHC Phase 4 (“30-Baht Treatment Anywhere”), revolutionizing healthcare access through digital systems. This initiative elevates Thailand’s 20-year-old universal coverage program by integrating nationwide telemedicine systems, centralized medical information systems, digital health platforms, and AI-powered diagnostics.
Pilot studies in Khon Kaen and Chiang Mai provinces demonstrate that this digital-first approach reduces waiting times by 63% and increases patient satisfaction from 74% to 89%, while lowering per-capita service costs by 22%.
Value-Based Healthcare (VBHC): Reimagining Cost-Effective Care
Thailand is emerging as a regional leader in adopting Value-Based Healthcare (VBHC) to address rising healthcare costs and improve care efficiency.
An example is the Phyathai–Paolo Hospital Group, which has successfully implemented VBHC principles to design personalized treatment plans and services tailored to individual patient needs. Under the VBHC strategy, the organization has significantly reduced overall costs and hospital readmission rates, demonstrating the tangible benefits of value-driven care.
Homegrown Innovations: Sustainable Healthcare Solutions
The National Health Security Office has implemented seven digital innovations in its Universal Health Coverage program:
- Telemedicine
- Medical Information Systems
- Health Technology Assessment (HTA)
- Personalized Medicine
- AI and Machine Learning
- Patient-Centered Medicine
- Integrated Health Services
These innovations have benefited over 105,000 patients nationwide, reducing treatment costs by 34% while elevating care standards. The WHO recognizes this success as exemplary for middle-income countries.
Technologies Reshaping Healthcare Delivery
1. Artificial Intelligence (AI): Transforming Diagnostics and Efficiency
AI is revolutionizing healthcare by enabling more accurate diagnostics, personalized treatment plans, and streamlined administrative processes. AI-powered imaging systems can identify diseases like cancer with up to 95% accuracy, significantly improving early intervention outcomes.
These systems complement rather than replace clinicians, allowing healthcare professionals to focus on the human aspects of care while AI handles data-intensive tasks. Massachusetts General Hospital’s use of AI in pathology has reduced diagnostic times by 30% while maintaining exceptional accuracy.
2. Telemedicine and Remote Monitoring: Healthcare Without Boundaries
Telemedicine has evolved from a pandemic necessity to a permanent fixture in modern healthcare, particularly benefiting underserved areas. Remote monitoring systems enable patients to manage chronic conditions from home, reducing hospital readmissions by 25%.
This approach proves especially valuable in rural regions with limited healthcare facilities. Ochsner Health’s digital medicine program for hypertension management has improved control rates by 21% while reducing emergency department visits.
3. Predictive Analytics: Anticipating Needs and Optimizing Resources
Predictive analytics empowers healthcare organizations to forecast trends and optimize resource allocation. From staffing projections to reducing readmission rates by 20%, this technology facilitates proactive decision-making that minimizes costs while improving patient outcomes.
When Geisinger Health implemented predictive analytics for resource planning, they achieved a 10% reduction in unnecessary hospitalizations and significant cost savings within the first year.
4. Blockchain: Security, Transparency, and Interoperability
Blockchain technology ensures data security and seamless information exchange across healthcare systems. By creating immutable records, blockchain fosters trust and transparency, enabling effective collaboration among providers.
Estonia’s national healthcare system demonstrates blockchain’s transformative potential, creating a secure and accessible health information exchange that has reduced administrative costs by 30% while improving care coordination.
5. Internet of Medical Things (IoMT): Continuous Health Monitoring
Wearable devices and IoMT technologies are transforming preventive care through real-time health monitoring. These technologies empower patients in self-management while providing clinicians with valuable data to improve treatment plans.
The Cleveland Clinic’s cardiac monitoring program using IoMT devices has reduced hospital readmissions for heart failure patients by 28%, demonstrating the significant impact of continuous monitoring on patient outcomes.
Measuring Enterprise Transformation Success
Healthcare organizations embarking on enterprise transformation should establish clear metrics to evaluate success:
- Clinical Outcomes: Improvements in patient health metrics, mortality rates, and quality indicators.
- Operational Efficiency: Reduced wait times, optimized resource utilization, and streamlined workflows.
- Financial Performance: Cost savings, revenue growth, and return on technology investments.
- Workforce Metrics: Improved retention rates, reduced burnout, and enhanced job satisfaction.
- Patient Experience: Higher satisfaction scores, increased engagement, and improved access to care.
Conclusion: A New Era for Healthcare
Enterprise transformation has evolved from an optional strategy to an essential lifeline for healthcare’s survival and prosperity. By embracing digital technologies, building resilient workforces, and adopting innovative approaches like Thailand’s UHC and VBHC initiatives, healthcare leaders can effectively address the twin challenges of workforce shortages and rising costs.
Organizations that commit to comprehensive transformation now will not only weather current challenges but position themselves as leaders in the next generation of healthcare delivery. The future of healthcare has arrived, bringing transformative potential to create more accessible, efficient, and patient-centered care systems worldwide.
Accelerate Your Healthcare Value Creation Journey
In today’s rapidly evolving healthcare ecosystem, digital transformation has transitioned from a strategic advantage to a fundamental imperative. Our study found that healthcare leaders who strategically integrate digital capabilities across their value chain are achieving operational resilience while delivering superior patient outcomes.
Organizations that leverage data-driven insights and implement end-to-end digital solutions are uniquely positioned to address the dual challenge of workforce constraints and escalating costs—creating sustainable competitive advantage in an increasingly complex landscape.
Discover how our teams can help your organization unlock trapped value, drive continuous innovation, and architect the healthcare delivery model of tomorrow.
Engage with our transformation strategists to explore your organization’s highest-potential opportunities.
📧 Email: [email protected]
📞 Phone: 02-636-7011
Sources:
- PubMed Reference
- ACHE Survey Summary
- Syntellis Report Summary
- Blockchain Case Study
- Thailand Case Study
- Frost & Sullivan Healthcare Market Research (2024)
- Ministry of Public Health, Public Health Resources Report (2023)
- World Health Organization (WHO) Country Statistics: Thailand (2023)
- National Health Security Office (NHSO) (2024)
- National Strategic Plan for Public Health 2024-2025
- Pilot Project Evaluation Report, National Health Security Office (2024)
- Annual Report of Phyathai-Paolo Hospital Group (2024)
- Universal Healthcare Coverage Progress Report, National Health Security Office (2024)






![Thumbnail [Post Event] HOW](https://bluebik.com/wp-content/uploads/2025/12/Thumbnail-Post-Event-HOW.png)